Having Achilles Tendon Repair Surgery
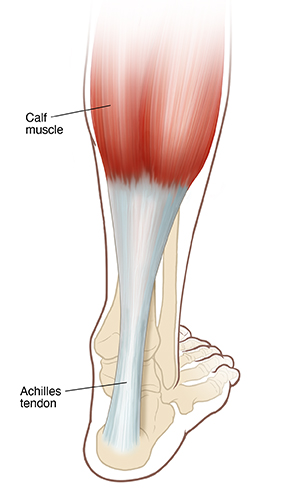
The Achilles tendon is a strong, fibrous cord in the back of your lower leg. It connects the muscles of your calf to your heel. It’s the largest tendon in your body. It helps you walk, run, and jump. Achilles tendon repair surgery is a type of surgery to fix a damaged Achilles tendon. The damage may be a tear or rupture from a sudden (acute) injury. Or the damage may be from overuse, or wear and tear, or from other conditions. This long-term (chronic) injury is also known as tendonitis or tendinopathy.
What to tell your healthcare provider
Tell your healthcare provider about any recent medical conditions and all the medicines you take. This includes over-the-counter medicines like aspirin and ibuprofen. It also includes vitamins, herbs, and other supplements. And tell your healthcare provider if you:
-
Have had any recent changes in your health, such as an infection or fever
-
Are sensitive or allergic to any medicines, latex, tape, or anesthetic medicines (local and general)
-
Are pregnant or think you may be pregnant
Tests before your surgery
Before your surgery, you may need imaging tests. These may include ultrasound, X-rays, or MRI.
Getting ready for your surgery
Your tendon repair will be done by an orthopedic surgeon. This is a surgeon who specializes in treating bone, muscle, joint, and tendon problems. Talk with your surgeon about how to get ready for your surgery:
-
You may need to stop taking some medicines, such as blood thinners and aspirin, before the procedure.
-
If you smoke, you may need to stop before your surgery. Smoking can delay healing. Talk with your surgeon if you need help to stop smoking.
-
Ask a family member or friend to take you home from the hospital. You can't drive yourself.
-
Plan some changes at home to help you recover. This is because you won’t be able to walk on your foot normally for a while. You may need help at home.
-
Follow any directions you are given for not eating or drinking before surgery.
-
Follow all other directions from your healthcare provider.
You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully. Ask questions if something is not clear.
On the day of surgery
The surgery can be done in several ways. Ask your surgeon about the details of your surgery. The preparation and surgery may take a couple of hours. During your surgery:
-
You may have general anesthesia. This is medicine that allows you to sleep through the surgery. Or you may have spinal anesthesia. This is so you won’t feel anything from your waist down. You’ll also likely be given sedation. This will help you relax and sleep through the surgery.
-
A healthcare provider will watch your vital signs, such as your heart rate and blood pressure, during the surgery.
-
The surgeon will make a cut (incision) through the skin and muscle of in the back of your calf. If you have minimally invasive surgery, the surgeon will make several smaller incisions instead of one large one. They may use a tiny camera with a light to help do the surgery.
-
Your surgeon will make an incision through the sheath or covering of the tendon. If the tendon is damaged, the surgeon may remove the damaged part and repair the rest of it. If you have severe damage, the surgeon may use muscle or tendon from your calf, ankle, or foot for the repair.
-
The surgeon will make any other repairs that are needed. They will then close the layers of muscle and skin with stitches (sutures).
A healthcare provider will watch you for a few hours after your surgery. When you wake up, you will probably have your ankle in a splint. This is to keep it from moving. Achilles tendon surgery is often an outpatient procedure. This means you can go home the same day. Sometimes you may need to stay overnight.
After your surgery
You will have pain after your surgery, especially in the first few days. Pain medicines will help relieve your pain. Keep your leg elevated as much as possible. This can help ease swelling and pain. Make sure to tell your surgeon right away if you have a high fever, chills, or pain in your ankle or calf that gets worse.
Your surgeon may replace your splint with a cast. Follow all directions about keeping your splint or cast dry. Or your surgeon may give you a special boot instead of a cast. The boot can be taken off. You will likely need to use crutches. This is so you can keep weight off your leg while the tendon heals. You may need help at home while you recover.
Make sure you keep your follow-up appointments. Usually at about 10 to 14 days after your surgery you’ll need to return to the surgeon to have your stitches removed.
Follow-up care
Your surgeon will give you directions about when you can put weight on your leg. They will tell you how to strengthen your ankle and leg muscles as you recover. You may have physical therapy to help with your recovery.
Make sure to follow all your surgeon’s directions about medicine, wound care, and exercises. This will help to make sure the repair is successful. If you have any questions or concerns, call the surgeon’s office.
When to call your healthcare provider
Call your healthcare provider right away if any of the following occur:
-
Chest pain or trouble breathing ( call 911)
-
Fever of 100.4°F (38°C) or higher, or as directed by your healthcare provider
-
Shaking chills
-
Splint or cast that seems too tight or too loose
-
Ankle splint, cast, or dressing that gets wet or soggy
-
Pale color or discoloration of the skin around the cast
-
Numbness or tingling near or under the cast or to the foot
-
Odor coming from the cast
-
Foot or toes that are pale, blue, or cool to touch
-
Pain that gets worse with or without activity
-
Painful calf that is warm to the touch and tender with pressure
-
Increased redness, tenderness, bleeding, or swelling of the incision
-
Drainage from or opening of the incision
-
Swelling in the foot, ankle, or calf that's not relieved by elevating the feet
-
Other signs or symptoms as directed by your healthcare provider